University Faculty Development Program (UFDP)
Welcome To
University Faculty Development Program RMU
We live in a momentous time, and the future calls for new paths and fundamental changes in medical education. The structure of medical schools has been influenced by an exponential increase in medical knowledge and changes in healthcare delivery, doctor availability and workload, patient expectations, and the needs and requirements related to students. To keep pace with changes, quality improvement and innovations in medical education are now being addressed by many important global associations and organizations, among them the World Federation for Medical Education (WFME), the Institute for International Medical Education (IIME), the American Medical Association (AMA), the Association for Medical Education in Europe (AMEE), the Canadian Association for Medical Education (CAME), the Association for the Study of Medical Education (ASME), the Association of American Medical Colleges (AAMC), the Accreditation Council for Graduate Medical Education (ACGME), the Australian Medical Association (AMA), and the Asia Pacific Medical Education Conference (APMEC). It is clear that a new vision is needed to address the challenges of medical education.
There is also a need for a new model to shape the minds and hearts of future healthcare professionals. This requires adoption of new curricula, novel pedagogies, and innovative forms of assessment, and, of course, even well-developed faculty members, since those individuals represent one of the most important assets of an academic institution.
To understand the importance of faculty members and their role in medical education, it is helpful to consider the relevant context. In general, medical education comprises three main components:
- A curriculum
- An educational environment
- Teachers/Faculty member
The curriculum concerns what is learned, how it is learned, how it is assessed, and how learning is structured. The teachers produce the course documentation in a process that includes discussing and learning together with other faculty members—a community of practice. The educational environment or climate has also been highlighted as a key aspect in this context 2-4, and both students and teachers are aware of that aspect of their university. Is the teaching and learning environment very competitive? Is the atmosphere in classes relaxed or in some ways stressful? These are all key questions in determining the nature of the learning experience 4. The importance of the environment should not be underestimated, and the interest in studying learning environments in health professions such as medicine has increased in recent years. One reason for that may be the growing diversity of both the student population and the student requirements.
Faculty members constitute the third major component of medical education, not only due to their direct influence on the teaching and learning process, but also because they play an important role in shaping the other two components (i.e., curriculum and environment).
Each of these three components has an important function in medical education, and, in combination, they can affect student achievements as well as the quality of the instruction provided, and hence they are also associated with the issue of patient safety.
Responsibilities of Medical University towards faculty members:
Medical Universities have obligations towards the faculty members, and those responsibilities can be divided into six categories:
- Recruitment
- Retainment
- Re-energization
- Recognition
- Rewards
- Respect
If a medical college is to succeed, it has to accept these responsibilities. The crucial role of faculty development activities and initiatives implemented at medical schools is clearly illustrated by this alarming statement made by Professor Ronald M. Harden 5:
“There is no such thing as curriculum development, only staff development.”
Thus faculty development is essential for ensuring and better addressing the obligations that medical schools have towards their faculties. Unfortunately, planning and introducing a faculty development program is not an easy task
Vision
To Provide Best Possible Patient Care.
To Inculcate the Values of Mutual Respect & Ethical Practice of Medicine.
Vision
To Provide Best Possible Patient Care.
To Inculcate the Values of Mutual Respect & Ethical Practice of Medicine.
Continuous Professional Development
In 2015, WFME published revised WFME Global Standards for Quality Improvement: Continuing Professional Development of Medical Doctors.6 These are a global medical education expert consensus on the best practice minimum requirements (basic standards) and standards for quality improvement. Altogether there are 76 basic standards, 62 quality development standards and 80 annotations.
Concepts of CPD:
CPD includes all activities that doctors undertake, formally and informally, in order to maintain, update, develop and enhance their knowledge, skills, and attitudes in response to the needs of their patients. Engaging in CPD is a professional obligation but also a prerequisite for enhancing the quality of health care. The strongest motivating factor for continuous professional life-long learning is the will and desire to maintain professional quality.
Continuing Medical Education (CME) describes continuing education in the field of knowledge and skills of medical practice; CPD, a broader concept, refers to the continuing development of the multi-faceted competencies inherent in medical practice, covering wider domains of professionalism needed for high quality professional performance.
WFME recommends the following set of global standards in CPD. The set of standards are divided into 9 areas and 32 sub-areas, being aware of the complex interaction and links between them.
AREAS are defined as broad components in the, process, structure, content, outcomes/competencies, assessment and learning environment of CPD covering:
- Mission and outcomes
- Educational program
- Assessment and documentation
- The individual doctor
- CPD provision
- Educational resources
- Evaluation of CPD activities
- Organization
- Continuous renewal
FDP-Concepts & Principles
The definition of faculty development has evolved and been expanded over the past few decades, and various definitions have been used in higher education. In 1975, Gaff referred to faculty development as the “activities that help teachers improve their instructional skills, design better curricula, and/or improve the organizational climate for education,” and, at about the same time, described as the broad range of activities used by institutions to renew or assist faculty members in undertaking their expected roles.
“Faculty development is a planned program or set of programs designed to prepare institutions and faculty members for their various roles”.
This broader and more inclusive definition has become generally accepted by the medical education community 8. Faculty development, or staff development as it is often called, has become an increasingly important component of medical education. Staff development activities have been designed to improve teacher effectiveness at all levels of the educational continuum (e.g. undergraduate, postgraduate and continuing medical education) and diverse programs have been offered to health care professionals in many settings.
It has been emphasized that medical school faculty members are trained in the roles of their discipline (e.g., clinical duties and healthcare delivery) but are essentially not taught to succeed as educators, researchers, scholarly writers, or administrators. In most cases, they do not learn academic skills related to curriculum development, instruction, evaluation, research, scientific production, or administration 7,8. Very few faculty members are trained to manage their roles as teachers 9. In addition, new tasks, as well as advances in medicine and new instructional techniques, often mean that old skills may be inapplicable or insufficient. On the other hand, the faculty members of today must acquire new competencies in areas such as information technology, evidence- based medicine, professionalism, problem-based learning, interdisciplinary teaching, web-based instruction, and new teaching strategies
Principles of Faculty Development
- Strong administrative support
- Reward structures for participation in faculty development programs
- Systematic skills development
- Based on principles of adult learning
- Sensitive to identified needs
- Participants learn from each other
- Atmosphere of caring and trust
- Based on collaboration, teamwork, and shared vision
- Celebration of successes
Need Assessment of Faculty Development
The academic vitality of any institution is linked with the professional development of its faculty members. Evidence shows that the most important asset of a medical school is its faculty and success of an institution is determined by the extent to which it invests and nurtures the career development of its most junior faculty members. Traditionally, medical school faculty members are hired only for their content knowledge and skills rather than for their teaching ability. However, it is increasingly being realized now that faculty members need to be trained in teaching and learning strategies to meet the demands of today’s, newer, more complex healthcare system
FD is imperative for all medical universities. It needs to be systematic and planned with an emphasis on newer evidence-based teaching strategies e.g. Work-based learning, e-learning and community-based learning. FD is an important institutional approach towards developing teaching excellence among faculty by promoting educational infrastructure, capacity building and collaboration and expertise sharing with international colleagues
Developing a system of incentives and awards for recognition of excellence in teaching, professional growth and research can help in motivating faculty to attend educational workshops.
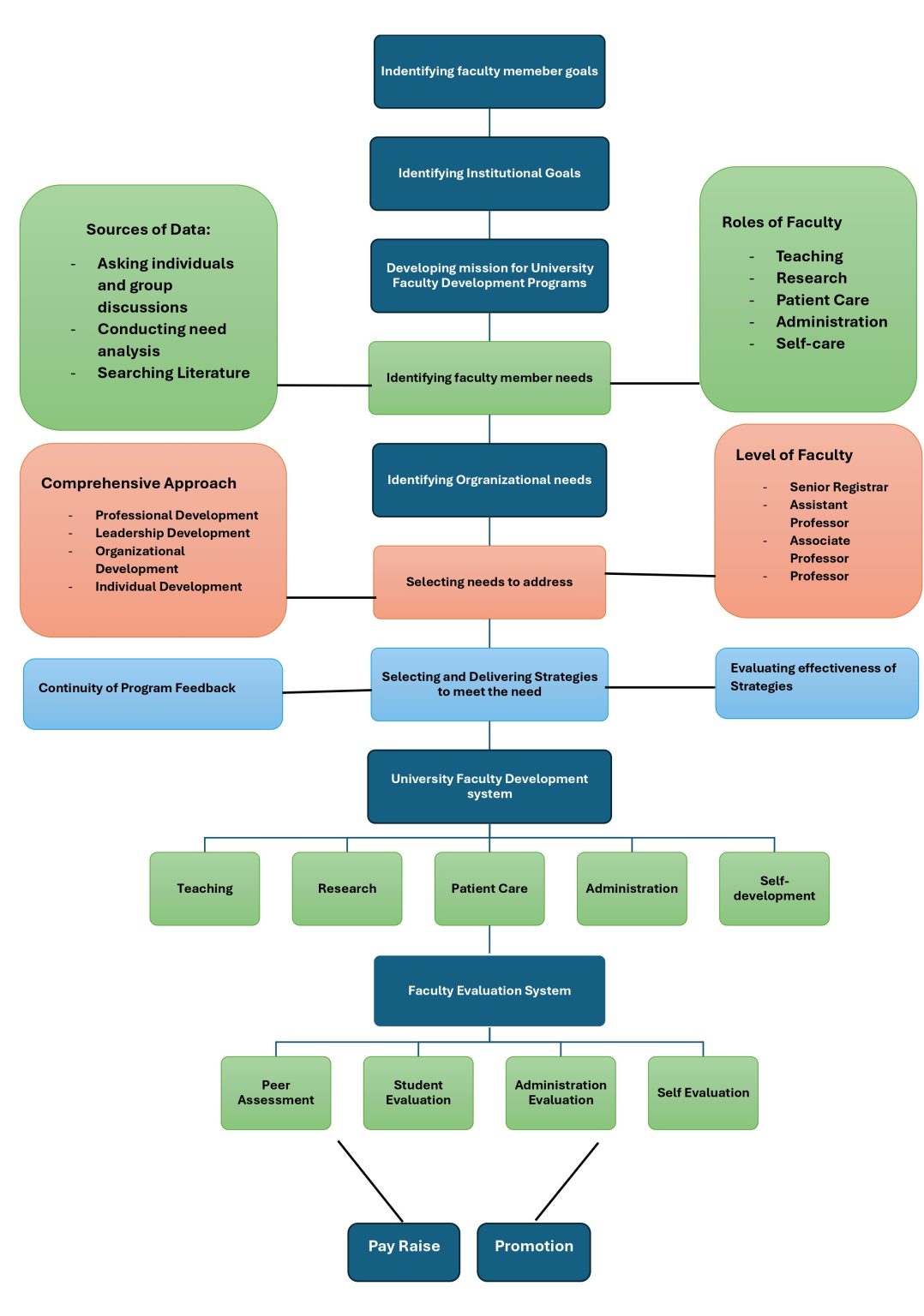
Framework of UFDP
In recent years, much emphasis has been placed on the importance of focusing faculty development programs not only on the needs of the targeted individuals, but also on organizational aspects. Effective faculty development has two important features: first, a broad perspective that continuously searches for and tries to address all the aspects that impact faculty success; second, systematic and rigorous attention given to each of the steps in the faculty development process. Therefore, when designing and implementing faculty development programs, it has been proposed that it is important to understand not only the objectives of individual faculty members, but the goals of the organization as well
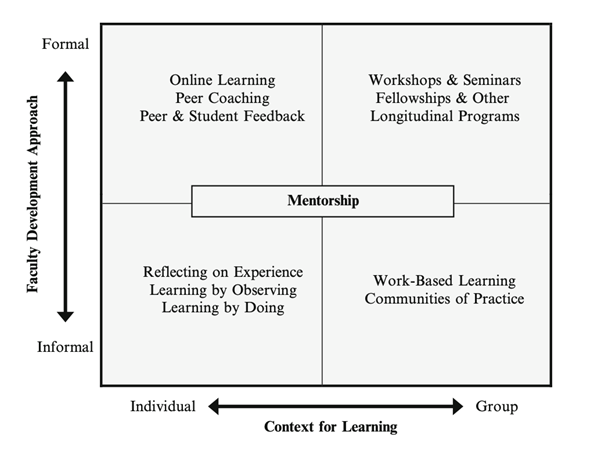
Model of Effective Faculty Development Program
An effective and comprehensive FD program should be built upon the following elements mentioned in BEME guide (Steinert et al. 2006).
- Professional development (new faculty members should be oriented to medical university and to their various faculty roles).
- Instructional development (all faculty members should have access to teaching-improvement workshops, peer coaching, mentoring, and consultations)
- Leadership development (academic programs depend upon effective leaders and well-structured curricula; these leaders should develop the skills of scholarship to effectively evaluate and advance medical education).
- Organizational development (empowering faculty members to excel in their roles as educators require organizational policies and procedures that encourage and reward teaching and continual learning).
- Program evaluation (FD activities appear highly valued by participants, who also report changes in learning and behavior. Certain elements of these activities appear to be consistently associated with effectiveness. Efforts are required to gather information from Participants about their satisfaction, learning behaviors/capability, and results or impact).
Domains of UFDP
A true faculty development program (FDP) ensures capacity-building in all the Five domains (Following WFME standards for CPD)
- Education (Instruction)
- Leadership
- Professional Development
- Personal Development
- Patient care
Faculty development has been expanded over the past few years in order to strengthen the academic base of institutions of higher learning. This has been done by providing different programs, which can be divided into those with the most common formats and those with alternative formats 12. The most common formats include workshops and seminars, short courses, sabbaticals, and fellowships, and the alternative formats comprise integrated longitudinal programs, decentralized activities, peer coaching, mentoring, self-directed learning, and computer-aided instruction.
Common Formats:
- Workshops
- Seminars
- Conferences
- CPC (Clinicopathological conference)
- Short courses
- Sabbaticals
- Fellowships
Alternative Formats:
- Integrated longitudinal programs
- Peer coaching
- Mentoring
- Self-directed learning
- Computer aided instructions
- Research
Steps in Designing UFDP
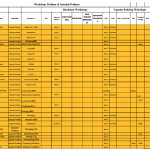
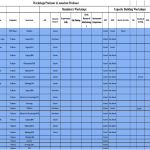
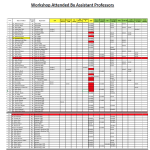
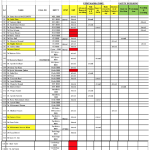
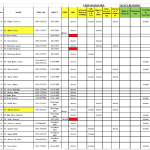
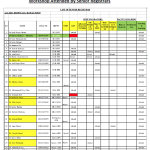
Rawalpindi Medical University is currently focused upon following major domains of continuous professional development.
Including:
- Clinicopathological conference
- Workshops/ seminars/courses
- State of the art guest lectures
- Curricular reforms
- Undergraduate
- Postgraduate
- International scientific conference
- National alumni
- International alumni
- Mentor ship dinner
- Rawalian’s reunion dinner
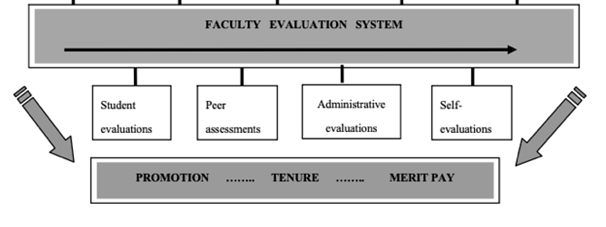
Faculty Assessment System
The aim of the assessment policy of the UFDP is to ensure that all submissions for accreditation receive appropriate assessment whereby all submissions are treated equally. By ensuring that all submissions are assessed thoroughly and consistently against the criteria required for accreditation.
Appropriate assessment methods would – besides traditional examination forms using norm- referenced and criterion-referenced judgments – include consideration of various tools for self-assessment, the use of personal learning portfolios or log-books and special types of assessments, e.g. site visits by peers, an agreed protocol and comparison with similar results of colleagues. It would also include systems to detect and prevent plagiarism.
Assessment requires:
- Credible data
- Trusted feedback
- A strategy for improvement.
Types of Assessment
Need Based Assessment
Formative Assessment
Summative Assessment
UFDP EVALUATION
“The purpose of evaluation is not to prove, but to improve.” Dr. Guba
In recent years, much emphasis has been placed on the importance of focusing faculty development programs not only on the needs of the targeted individuals, but also on organizational aspects. Effective faculty development has two important features: first, a broad perspective that continuously searches for and tries to address all the aspects that impact faculty success; second, systematic and rigorous attention given to each of the steps in the faculty development process. Therefore, when designing and implementing faculty development programs, it has been proposed that it is important to understand not only the objectives of individual faculty members, but the goals of the organization as well.
An essential component of professional development activities involves ongoing and systematic evaluation procedures. Few efforts have been made to evaluate the results of professional development beyond the brief responses requested at the conclusion of workshops which assess participant reaction to the session. It is an especially critical time for the adult education field to emphasize the evaluation of professional development for at least two reasons:
- Given the certainty of diminishing resources and competing priorities, the luxury of unfocused and unexamined professional development no longer exists. Increasing participation and financial support by non-educational partnerships are bringing to adult education new demands for accountability.
- If adult education practices are to respond to rapidly changing technological and social structures, professional development is the primary vehicle for meeting that challenge. Sound information is needed to make thoughtful decisions on how to change direction
Evaluation of the impact of professional development activities must address the following two questions:
- Does professional development alter long-term instructional behavior?
- How do we know that professional development activities do, in fact, improve learner performance?
CME / CPD Requirements
Requirement of credit hours:
The guidelines had been given by PMDC:
- 5 credit hours-years of CME training from a recognized professional body is mandatory for general practitioners.
- 10 credit hours-years of CME training from a recognized professional body is mandatory for
- No carry-forward of extra credit points is acceptable after 5
Guidelines for Credit Hours:
Here we set the criteria for accreditation of CME hours according to following PM&DC rules.
- One Credit Hour is equal to 3 clock hours
- Maximum 6 hours duration per day shall be 2 credit hours.
- Speakers at any conference, CME, CPD, workshop, or training program will be given one credit hour per lecture given. If they attend the whole CME/CPD as a delegate, then they will be given the approved points of the CME/
- The doctors may attend the international CME/CPD conference held overseas on the production of the certificate of attendance. CME/CPD credit hours will be given as per the equivalence formula.
- The institutions should be accountable for deciding/labeling credit hours for each activity, as the degree of assignment of candidates varies with the type of activity, e.g., lecture, workshop. The level of competency achieved in one-hour session for a skill training workshop is different from the one achieved through a one-hour